summary heart failure talks
thanks to Safras and Mohamed for the talks on heart failure
Below is a summary of take home points
1) new guidelines are out on Heart failure ( nice guidelines ) as of OCTOBER 2014- click on image above for link to FREEDOWNLOAD
. These guidelines are 100s of pages long and reflect the opinion of 100s of clinicians , researchers and patients
. These guidelines are 100s of pages long and reflect the opinion of 100s of clinicians , researchers and patients
There is a de-emphasis on NIV and GTN which doesnt reflect our real world. This is not the fault of the guidelines because neither treatments have much effect on long term survival . I dont believe we can prove their efficacy in terms of short term survival because it would be unethical to do RCTs that involve withholding these treatments on patients in distress in ED
The take home points ( their best interpretation of evidence and expert advice )
Heart failure is the the commonest cause for hospital admissions to hosptial in the over sixty fives
Acute Pulmonary Oedema – is the commonest True ED emergency related to heart failure . The blood pressure is preserved or even high ( I find the pathophysiology behind this hard to fully understand as the usual causes such as mi or Ischemia are not culprits . It is said that there is often a diastolic component , so these patients often have the risk factors for diastolic dysfunction such as diabetes and hypertension )
Assessment
1) acutely the main things are a preserved or high blood pressure and wet lungs ( creps) . When this clinical finding is not obvious ( eg in an obese patient with a history of COPD or risk factors for PE ) , bedside ultrasound has a new and crucial role
Treatment
2) traditional approach is oxygen , frusemide , morphine , nitrates and consider NIV
3) a more rational priority ( and reflective of current ED Practice ) is
Oxygen – best given via NIV ( whatever you have BIPAP or cpap )
Frusemide – standard iv dose ( doesn’t really matter what that is but usually the patients oral dose is given iv)
Gtn ( given first under the tongue 2 sprays = 400mcg) and then as an infusion starting high and lowering if patient becomes hypOtensive eg start at 100mcg per minute or even more ( double this )
congestive heart failure with preserved blood pressure
Assessment.
The crucial points about diagnosis are BNP and a good clinical exam with good basic tests ( ecg/cxr/labs) . The patient should then get an echo (best as in patient ) and this should be a formal one as valvular heart disease needs to be ruled out and this is not yet in the domain of a basic ed bedside echo. Of course it would not be unreasonable to assess EF on bedside echo eg by eye ball estimation or EPSS
Important Inpatient recommendations and guidelines
1) The need for heart failure patients to be linked in to Specialist Clinics
This is an evidence based recommendation and may be because all the things that comes with specialist clinics eg attention to detail / community outreach etc and addressing risk factors :
– dietary and life style measures
– blood pressure / cholesterol / weight / obviously smoking sessation
medication
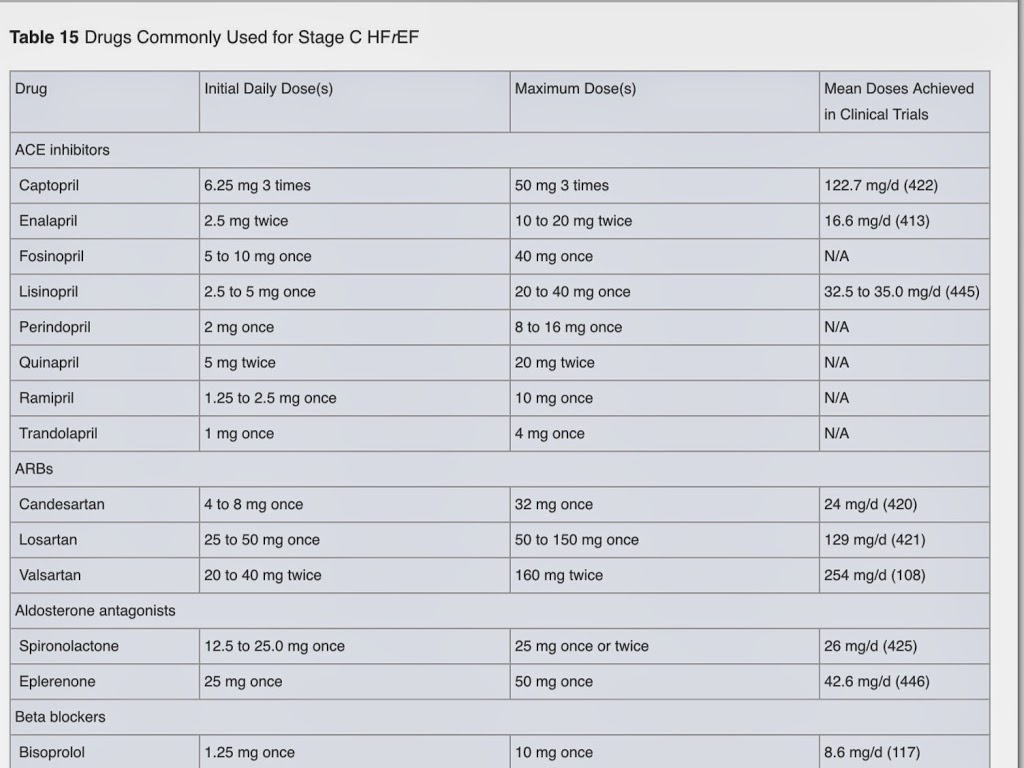
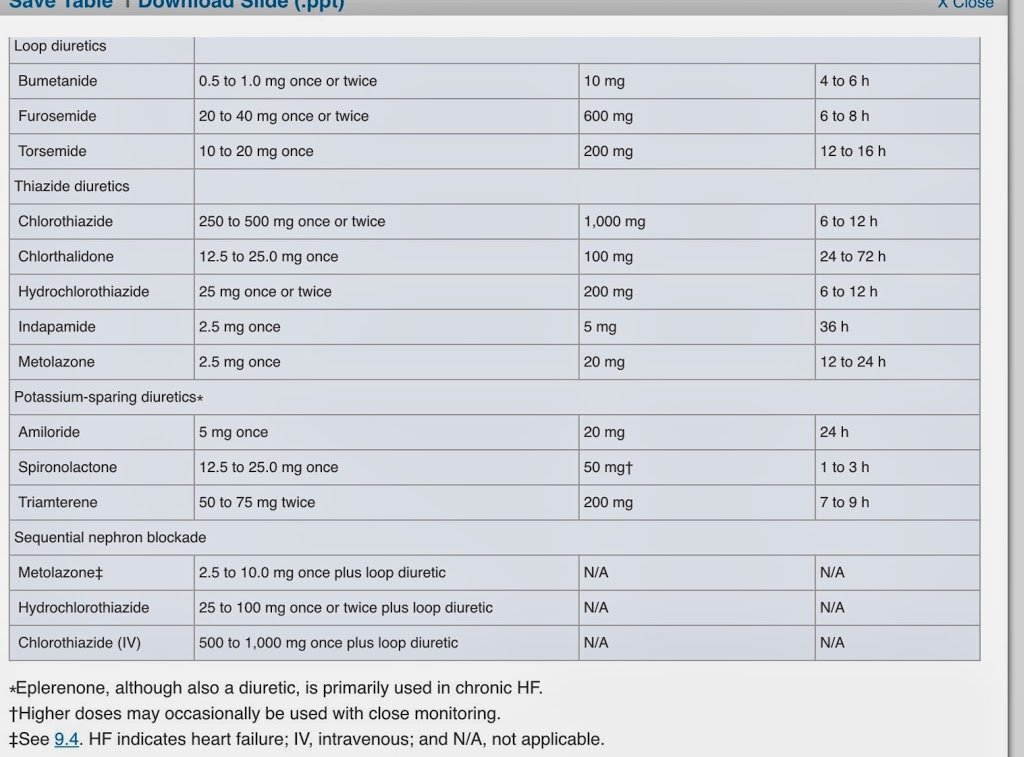
See table attached below of appendix in guidlienes about drug doses
take home points
– give an ace inhibitor ( or equivalent … if possible ) -eg start enalapril 2.5 mg daily and get GP to oversee increments up to ……..
– add a betablocker if patient is stable .that means out of ED , off iv diuretics etc . cardivolol / metoproplol succinate / bispoprolol being evidence based . Better to add a betablocker than increase dose of ace inhibitor according to the guidelines . eg bisoprolol 1.25 mg daily increasing over weeks to
– if giving a betablocker add a thiazide as ankle swellling is a problem
Persistent uncontrolled nyhc grades 2-4 :
– add in spironolactone ( or equiv anti aldosterone equivalent ) —eg
– add in digoxin —
FINALLY
tNOT INCLUDED IN THE NICE GUIDELINES THE COOL STUFF
1) ULTRASOUND
Bedside ultrasound really has such a useful and now evidence based role to play in acute assessment not the least of which includes
IVC assessment when fluid loading
left heart gestalt EF estimation and EPSS
lung assessment – lung rockets or B lines and response to therapy
rule out right heart strain
2)
The high end stuff -REBOA / AORTIC BALLOON COUNTER PULSATION