ED THORACOTOMY
thanks Karen for a great talk on ED thoracotomy
Here are some of the take home messages and references
1) Penetrating stab wounds to the chest ( particularly in the area of the left parasternal /precordial area) are the sort of patients that may come to ED and having suddenly lost an output and need consideration for ED thoracotomy .These patients DO survive , commonly !
2) the ED thoracotomy is performed in the periarrest situation where the patient cannot be taken to theatre in sufficient time . If the patient can be taken to theatre ( because he has a perfusing circulation ) then an Emergency Thoracotomy should be performed there instead .
3) penetrating stabs are the ones that may ( and often do ) survive. Blunt trauma is unlikely to survive ( < 1%) chance if they go into arrest in ED. A patient with blunt trauma and cardiac tamponade who goes into arrest in ED could be considered for thoracotomy in ED . A patient with blunt trauma and massive Heamothorax who goes into arrest (and without a tamponade ) will not survive unless the person opening the chest can manage hemorrhaging mediastinal vessels ( and that just is not us in ED )
4) it would be considered worthwhile to attempt ED thoracotomy on a balllistics injury to the chest if there is evidence of tamponade in a patient who loses output on arrival . If there is no evidence of tamponade then ED thoracotomy should not be done unless there is a surgeon there who is willing to help ( stop catastrophic mediastinal vascular injury )
summary
1) make the decision that ED Thorocotomy (Be very clear of the indication and what you intend to do once you open the chest )
2) WHO DOES It? surgeon if he has experience and is there , if not the most senior ED doctor (hope its not me )
3) This is a periarrest scenario so no time for niceties – use poviodine if its there and protect yourself and your staff with appropriate surgical gowns and possibly eye gear
4) during the periarrest situation there should be someone managing the Airway and intubation ( RSI with or without sedation and paralysis ) and there should also someone managing access ( IO / rapid transfuser / activating MTP etc ) .ALTHOUGH CONTROVERSIAL TAMPONADE IS STILL TREATED WITH FLUID LOADING AS PRELOAD WILL HELP OVERCOME FORCE OF TAMPONADE
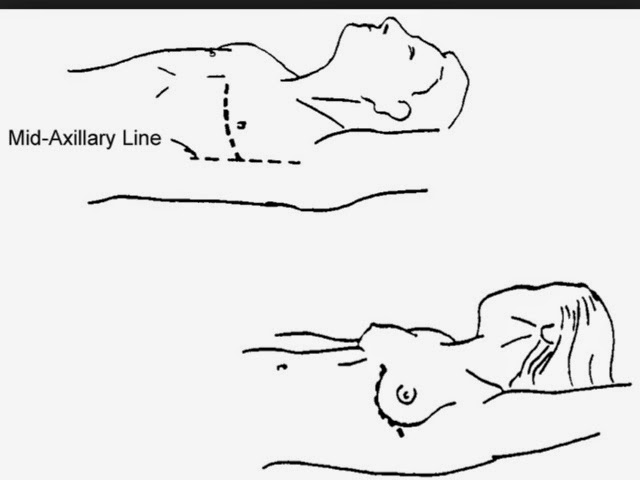
5) the third doctor who may be the team leader : cut at or just below where the nipple line would be if the patient were a skinny male . Cut deep to fat and right down to intercostal ligament and either cut right down through pleura oruse a blunt dissector of this ( this is a life saving emergency so speed is of the essence and cutting right down to lung would be considered acceptable ) . Be aware of two possible sources of iatrogenic bleeding , this would be the intercostal areteries running below the rib and the internal mammary arteries running parallell and close to the sternal margin. So if you are cutting so deep the Mantra ” above the rib below is of importance
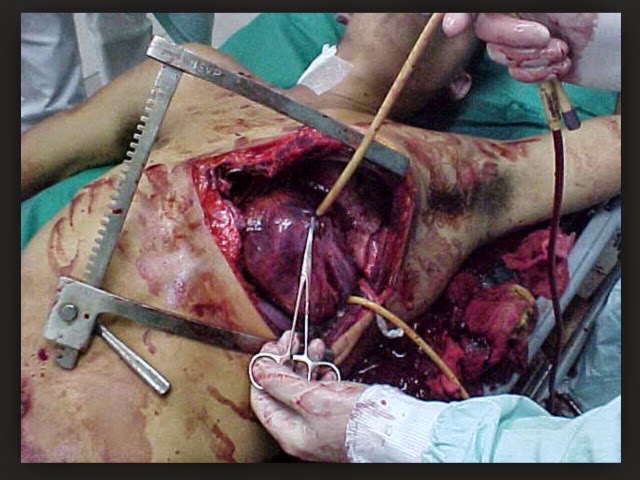
6) The pericardium should be immediately exposed by this and the lung automatically collapsed and out or the way .The ribs are held back by the rib spreader . IF the pericardium is not exposed then continue the cut across the sternum and to the otherside (clam shell )
7) Divide the pericardium using forceps ( Beware of cutting the phrenic nerve – this should be visible on the pericardium ) . Look for a ventricular hole and suture it , put a finger on it , put a Foley catheter baloon through it and inflate it DO ANYTHING !
8) the patients heart may need to be restarted and hand cardiac massage may need to be performed (two hands ) during much of this period ( use paddles only 20-30 joules necessary )
9) if you have managed to gain a perfusing blood pressure then the patient needs to go to theatre and this needs to be in sligo , regardless of the expertise of the surgeon on call . He can be stabilised more before definitive transfer